It can be so frustrating to be stopped in your tracks by an IBS flare up. Perhaps your belly has swelled up so you look pregnant, or you’re rushing to the loo every 10 minutes so can’t leave the house. These are all things my clients struggle with.
Read on for my tips on how to calm your body and mind during an attack of your irritable bowel.
What is an IBS flare up?
An IBS attack is an increase of your digestive issues. Irritable bowel syndrome can often come and go. A sudden rise in bloating, gas, diarrhoea or constipation can be triggered by something you ate, anxiety or stress, medication, alcohol, or changing the way you eat.
Some people get a flare-up regularly, other people can have long gaps between their IBS flare-ups.
How do you calm IBS?
The best thing to do during an IBS flare up is to look after yourself and take some time out to recover. Of course, rest might not be so easy to actually put into practice when you’re busy and have caring responsibilities.
The following ideas may help you relieve your IBS flare-ups next time your digestion kicks off:
- Heat packs or hot water bottles on your stomach can ease pains or feeling of sensitivity
- Try drinking some soothing teas for digestion – Read about the Best teas for IBS
- Wear comfortable clothes with a soft expanding waistline to accommodate any bloating
- Take a warm bath to help yourself relax and soothe your stomach
- Snuggle up in bed and allow yourself to rest whenever you can
- Try some gentle movement to help ease gas and stomach pains
- Eat low FODMAP foods for a few days to ease your way through the flare (see below for more on how to do this).
Read more >> about the low FODMAP diet for IBS – The beginners guide to the low FODMAP diet
There isn’t a ‘one pill cure’ for an IBS attack like some health conditions, so unfortunately you may need to try a combination of these activities to see what works for you.
IBS Flare up top tip – I’ve found that clients who combine some basic self care, some gentle movement and diet changes tend to calm the flare up more quickly.

What causes irritable bowel attacks?
The most frustrating thing is, that even when you are doing everything ‘right’ you may still get an attack of IBS.
The flare could be caused by eating something that didn’t agree with you, or something that happened to stress or upset you. Sometimes it’s not related to what you’ve been eating at all!
I find most of my clients start by blaming the last food that they ate. Of course, this seems to make sense that the most recent food could be the cause of your bloating or dash to the toilet.
But, did you know it could also be related to how you’re feeling?
We know that our mental state has a large part to play in digestion.
- Stress – When we’re stressed we will have less energy for digestion, which means foods aren’t broken down as well by the process of digestion, so they cause bloating and sensitivity. This could be coupled with pain, and either diarrhoea or constipation. When you’re not feeling calm, your digestion won’t be calm either!
- Lack of sleep – when we’re tired we feel more pain so you may be more sensitive. We also tend to eat more sugary, carb heavy foods when tired which can affect gut health. Related post – Sleep and Gut Health
- Diet – Eating something that doesn’t agree with you can cause an IBS flare up – this will be different for everyone, but could be too much fibre, coffee, alcohol, sweeteners, dairy, high protein diet, very greasy foods, or processed foods.
- Menstrual cycle – women may find IBS symptoms worse just before or around their period. This is because the hormones that make the uterus contract to release the lining, also affect the intestines which are nearby. This can lead to more cramps and pains.

Get the Ultimate Low FODMAP Diet Guide
Follow my step by step process, with 2x tasty 7 day meal plans, checklists, assessment kit.
What to eat during an IBS flare
Some of my clients find that eating a low FODMAP diet can help. FODMAP is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols. These are types of fibre and starch that can be fermented in the gut.
You might find foods lower in fermentable carbohydrates during a flare up of IBS can improve symptoms like bloating, gas and pain.
FODMAPs are in common healthy foods, but in some people with IBS they can cause bloating, gas, cramps or diarrhoea. Typical high FODMAP foods are onions, garlic, wheat, mushrooms, red pepper, beans and lentils, stone fruit such as peaches and cherries, and dried fruits.
What to eat during an IBS attack – Example low FODMAP foods you CAN eat includes chicken, tofu, oats, eggs, kiwi, melon, potato, rice, blueberries, broccoli and many more.
I find some of my clients struggle to put a selection of low FODMAP foods into a normal meal, so I created the 7 day low FODMAP Meal plan. Try it for a low FODMAP selection of healthy recipes.
It’s not a diet to be followed long term, but can help in the short term during an episode of IBS. Eating a low FODMAP meal won’t instantly calm your symptoms, but it can take the pressure off adding more gas and bloating. You need to keep eating, so avoiding adding additional fermentation might help relieve your discomfort.
How long does an IBS flare last?
Everything with IBS is very individual but you should experience an upset stomach for around 1-4 days before things settle down again.
If you’re not getting better, and the IBS flare up seems to be lasting for longer than usual you may need to speak to a doctor to confirm there is nothing else going on.
What does an IBS flare up feel like?
Your IBS attack may include:
- bloating or swelling in your tummy
- excess gas (with or without odour)
- diarrhoea
- constipation
- abdominal pains
- feeling sensitive around your digestion
- feeling like you haven’t been able to fully empty bowels
Some people might get an IBS attack once a week or more frequently. On the other hand some people might only get a flare up every few months.
Get the Ultimate Low FODMAP Diet Guide
Follow my step by step process, with 2x tasty 7 day meal plans, checklists, assessment kit.
What foods could trigger an IBS attack?
Some foods higher in fermentable fibres, sometimes referred to as FODMAPs, can trigger bloating, gas and diarrhoea. Common foods such as wheat, lentils, apples, mushrooms, dates, cashew nuts, onion, garlic, asparagus and avocado are all high FODMAP foods.
FODMAPs are fibres or sugar alcohols which don’t get broken down in the small intestine as normal.
This poor digestion leads to water being drawn into the small intestine which can feel like bloating, or diarrhoea. Alternatively the molecules of partially digested foods can travel to the large intestine, where they are fermented by gut bacteria. The fermentation causes excessive gas, or you may also experience the movement of more water into the colon, causing diarrhoea.
If you eat a large amount of these foods in one meal they may contribute to your IBS episode.
Other common foods triggers for an IBS attack can be high amounts of caffeine, or alcohol, or a high fat meal.
- Caffeine speeds up gut transit time which can cause diarrhoea or cramps. Caffeine in tea, coffee, energy drinks or even chocolate, and can also increase feelings of anxiety which may contribute to digestive issues. Limit your intake to 1-2 cups a day, or even try cutting it right out of your diet.
- Alcohol is known to cause to irritation to the gut lining, and it’s not only during drinking that you can experience gas, loose stools or cramps. It can sometimes upset your digestion for a few days, so think about how much you’re drinking, and how often.
- High fat meals – when we eat meals with lots of saturated fats it can affect IBS in two ways. Firstly, if you don’t digest fats properly you might find you get diarrhoea. Signs of fat malabsorption include frothy stools, particularly light coloured orangey poo. Alternatively, you may find high fat meals slow down your digestion which can create more fermentation and gas.
Over the counter help for IBS flare ups
Your pharmacist may be able to provide help for dealing with flare-up symptoms like bloating, constipation, gas and diarrhoea.
Some products you might find helpful to deal with a flare-up include:
Laxatives
- To encourage a bowel movement, some work within 5 hours, some take a few days.
- You can try different types of laxatives to find a solution that works for you. Some laxatives provide more fibre which adds bulk to the stool, and hopefully stimulates the need to go. Other laxatives draw water in the large intestine to soften the stool, or cause the intestines to contract. It’s ok to use a combination of products for a short while during a flare up, but check with your doctor or pharmacist if you have questions.
Anti-diarrhoea meds
- Useful to control loose stools.
- Short term use is fine.
Peppermint Capsules (e.g. Buscomint, Colpermine)
- Useful for cramps and gas
- Look out for ‘enterically coated’ or ‘sustained release’ to avoid burning sensation and / or reflux. Enterically coated means the capsules will only open in the alkaline environment of your small intestine, rather than the stomach.
Products to disperse the wind (e.g Simeticone)
- These contain an anti-foaming agent by changing the surface area of gas bubbles causing them to come together to move through the gut. The medicine isn’t absorbed
Antispasmodic (e.g. Buscopan)
- Useful for cramping and pain, and should work within around 2 hours.
- Not to be taken with constipation (because they slow down motility of the gut (the opposite of what you want!)
If you’re ready to identify what triggers your IBS flares, and find ways to calm them, then please get in touch.
I can help you, as I’ve helped many other people already find a diet that works. Send me a message to get started on your IBS Gut Reset.
Check out a few Frequently Asked Questions on IBS flares:

IBS Nutritionist
Hi, I'm Anna Mapson, registered Nutritional Therapist.
I help people with IBS and SIBO get control of unpredictable gut symptoms to find long term relief from painful and embarrassing IBS without restrictive dieting.
I can help you to:
- understand your digestion better, so you recognise your triggers
- eat a well balanced diet, with tasty meals that are simple to prepare
- reintroduce your trigger foods so you can get back to enjoying food again
Find more about my 3 month 1:1 Gut Reset programme.
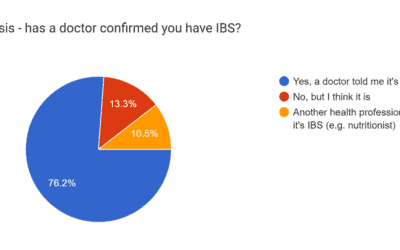
The impact of IBS on daily life
The struggles of IBS: A new survey reveals the profound impact on daily life. I ran a survey with my audience about the impact of IBS, and the way Irritable Bowel Syndrome (IBS) affects your day-to-day lives is really clear. I already knew from my work with clients...
Taking amitriptyline for IBS
Have you been offered a low dose of amitriptyline for IBS? It's a antidepressant that's sometimes offered to patients who experience significant abdominal pain related to digestion. If you're unsure about taking medication for your IBS, you're not alone. I hear this...
Why breakfast is important if you have IBS
Is breakfast the most important meal of the day? Many people I work say they just don’t feel hungry in the morning, and so avoid eating. Maybe you don’t want to start off your bloating that hits as soon as you eat. Or you feel a bit nauseous first thing and want to...




I am looking for advice with out having to pay for a ton of food I will not eat. I am a picking eater and hate textures so I am looking for ways to put things in my diet I can handle
Hello Nina it sounds like you need some individual support to find a diet that will work for you, please get in touch to arrange an appointment with me. My 3 month Gut Reset will do this, as well as supporting you for 3 months with your food choices so we can hopefully expand your range of meals. You can read about my way of working here: https://www.goodnessme-nutrition.com/consultations/ I recommend booking a quick call to speak to me first using the Contact page.
I have celiac and have been gluten free for 7 months, without feeling much better. Was told now it’s ibs causing symptoms. I’ve tried low fodmap to an extent but my triggers are both high and low fodmap, with most everything I eat. My “flare” if that’s what you want to call it, never goes away! I’m interested in finding out your rates and about your program.
Hi Brandy, you can read more about my programme and rates here and please do contact me about working together if you’re interested in getting some support with your diet. https://www.goodnessme-nutrition.com/consultations/
HI Anna I got IBS for 10 years reach
Ready Meals help me in supermarkets next day in the morning I was pain go out for work
2 days I know which food have & snacks